
Did you know that you are constipated if you go only once per day, if you don’t feel empty after a bowel movement and if you strain in order to go?
In scientific terms, constipation is a disorder in the gastrointestinal tract, which can result in difficult stool passage with pain and stiffness and infrequent stools.
Constipation is very common nowadays (more processed diets, more medications, and sedentary lifestyles) and most people are affected at least at some point in their life. Constipation is accompanied by nausea and/or bloating in some people, as well as great discomfort.
The long-term effects of a slow bowel include fissures, haemorrhoids, faecal impaction and rectal prolapse. Diverticular disease is another one. It happens when small hard stools lead to increased intestinal contractions, creating pressure which leads to the formation of a little pouch of the intestine. Acute constipation can even lead to the closure of the intestine, which may even require surgery.
The quality of life, general health, social functioning and mental health can all be significantly affected by chronic constipation. The main difference between functional constipation and IBS is the pain and discomfort that accompanies IBS. Less commonly, constipation is caused by a large/dilated bowel, a condition called megacolon.
Many people suffer in silence and try to self-medicate, while for those who do seek help, treatments can be unsatisfactory, superficial and often worsen the problem. The cost of constipation on NHS is estimated to be £81 million per year, without taking into consideration GP visits and OTC laxatives!
Primary constipation (the one that occurs without any clear cause) can be further classified into normal transit, slow transit or pelvic floor dysfunction.
With normal and slow transit, there may be functional obstruction in the form of dysfunction of pelvic floor and anal sphincter muscles.
IBS-C occurs when there is difficulty with bowel opening and abdominal pain associated with going. It can be made worse with stress or depression.
Slow transit is when the muscles of the intestine stop working properly.
If you google “Bristol Stool Chart” you will see a chart of different forms of stool. The form can differ because each one of us different place of living, gut flora, health history and lifestyle. In general, types three and mainly four are healthy, and five can be healthy in vegetarians.
The most common causes we look at are:
It is important to check for low stomach acid when constipation is present. There are many tests that can be used with your practitioner (zinc test, digestive enzymes, baking soda test…)
Ginger, apple cider vinegar, lemon, good hydration between meals, eating when relaxed, fermented drinks and veggies, bitter veggies, and eating protein at the beginning of the meal can all help with hypochlorhydria.
Due to the decline of oestrogen and progesterone and the rise of cortisol, coupled with weakened pelvic floor muscles, constipation is quite common in menopause. On the other hand, 16-OH oestrogen metabolite, the one that protects the bones, depends on a good bowel movement.
Our job is to improve hormonal levels while working on the different causes of constipation.
There are many different types of iron. Usually, the ones prescribed and the cheaper ones cause gut issues, including constipation. Iron fumarate and bis-glycinate are bioavailable, and hence less likely to cause any digestive issues. This is especially true when they are coupled with vitamin C and probiotics.
Chronic constipation is almost always caused by intestinal dysbiosis, usually because of a lack of bifidobacteria.
A comprehensive stool analysis or microbiome test and SIBO test can be very valuable in successfully addressing the causes of constipation.
T steady build-up of prebiotic fibres, mineral balancing (like magnesium) and neurotransmitter balancing (seotonin, GABA) are all important in addressing most types of constipation.
Laxatives and suppositories are not recommended, especially for chronic constipation. You quickly build a tolerance to the initial dosage needing a higher and higher dosage. A dependent bowel will become a lazy bowel. Also, laxatives come with side effects such as pain, diarrhoea and lack of nutrient absorption. Before knowing it, you are trapped in a vicious cycle.
The Western raised toilet is a relatively modern invention! But the puborectalis muscle in our pelvic floor is in a constant state of contraction to maintain continence when we stand and sit. When we squat, the muscle relaxes and the rectum strengthens which lets gravity do the work for us. Instead of squatting, there are ways to mimic this position, like a stool placed under our legs.
The vagus nerve is the primary component of the parasympathetic system (“rest and digest” vs “fight or flight”). A strong vagal tone promotes gastric juices and digestive enzymes, good peristalsis, a healthy microbiome and intestinal integrity.
Many exercises can activate the vagus nerve, for good peristalsis, including gargling, gagging, breathing exercises and good posture.
Adding more healthy fats and oils to the diet increases bile acid release.
Eat complex carbohydrates and starches, like vegetables, root vegetables, fruits and a few whole grains (or other fibres if you are on a Paleo/Keto diet), bran and some helpful fruit like kiwis or prunes. Following a low-carb diet for too long can affect the thyroid and adrenals and hence bowel motility. People with sensitive guts need an increase in soluble but not insoluble fibre. Your practitioner will guide you, depending on your individual symptoms.
Supplements are very important in the restoration of gut health and motility. Your practitioner will make sure you are taking all nutrients necessary (from diet and if needed from nutritional supplements) for good bowel functioning.
We cannot address constipation (or any gut issue) in a one-size-fits-all approach. Constipation and IBS need to be approached in a personalised way. Before jumping to solutions, we need to identify the underlying factor(s) and address them accordingly.
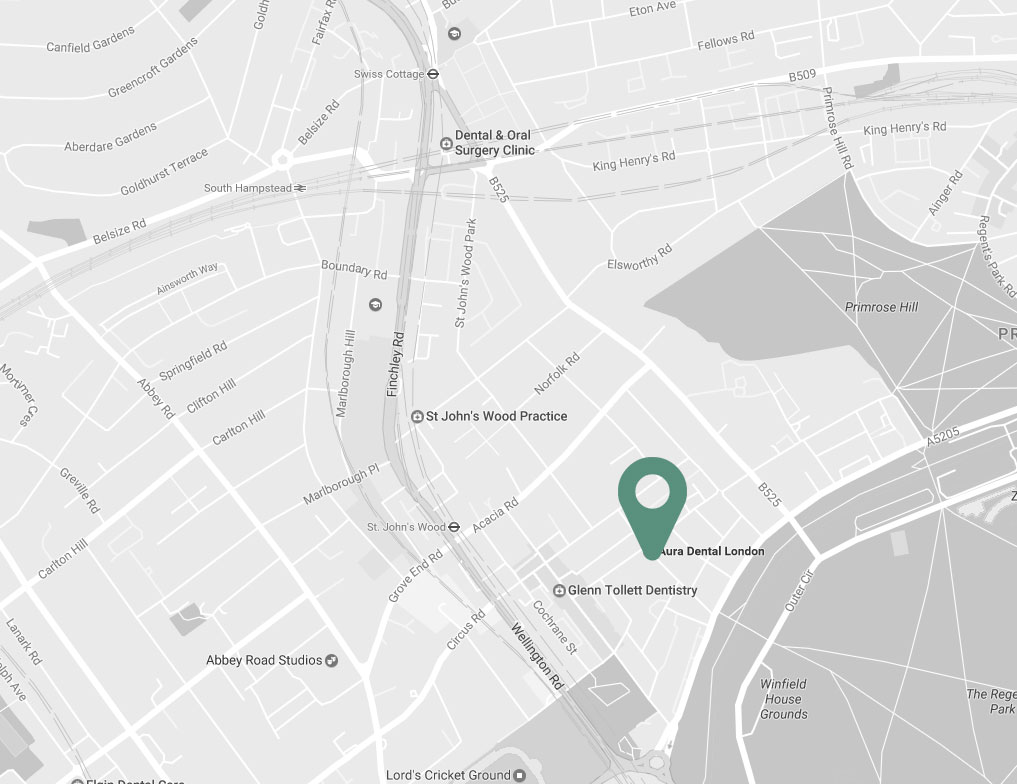

| Charlbert St, St John’s Wood London NW8 7BT |
|
| +30 6977 2099 88 | |
| info@naturopathy-med.com |