
One of the most common complaints I get in my clinic is chronic fatigue and low energy levels. While this is common, it is not normal.
Many people wake up unrefreshed, tired and are unable to finish their daily tasks because of unexplained tiredness. This can have a great impact on work, social relationships and family.
The failure to address chronic fatigue is due to the fact that it is a multifactorial issue. Energy production is complex and depends on many factors.
A detailed case history and, if needed, one or more functional tests can shed light on the factors that suppress the body’s ability to produce energy and can greatly improve quality of life in the great majority of cases.
Fatigue is a normal sensation that occurs after significant body activity, usually towards the end of the day. Fatigue is a signal that the body needs to rest, repair and regenerate for the next day. However, more and more people feel that rest and sleep are not enough in order to have optimal energy levels in order to accomplish all of their tasks and responsibilities.
We wake up tired, stressed, feel apathetic and sleepy, struggle to focus, have less than optimal memory and cognitive clarity. We often feel irritable because of fatigue and the body’s increased effort to meet its daily responsibilities.
90% of the energy that our body needs is produced in organelles inside cells that are called mitochondria. Every cell has thousands of mitochondria.
Mitochondria’s role is to convert nutrients from food to energy. A complex system of chemical reactions that take place in mitochondria, produces stable energy. When the system gets inefficient, we progressively feel less energetic and unrefreshed from sleep.
Low energy production that is due to mitochondrial dysfunction, is a significant factor in the manifestation of chronic disease, like autoimmune conditions, cardiovascular disease, cancer, obesity and diabetes.
The major factors that lead to mitochondrial dysfunction are the following:
Coenzyme Q10 is often prescribed in chronic fatigue. However, it is only one of the 30 micronutrients that mitochondria need for optimal function.
Functional testing can identify the level of mitochondrial dysfunction, by measuring metabolites that get accumulated when chemical reactions don’t occur. These chemical reactions depend on specific nutrients. This is the most accurate way to measure nutrient needs.
By doing this, you can cover the body’s needs in nutrients, and address metabolic dysfunctions and energy levels. As a result, life quality can improve a lot.
Based on clinical experience, restoration of energy-yielding mechanisms leads to:
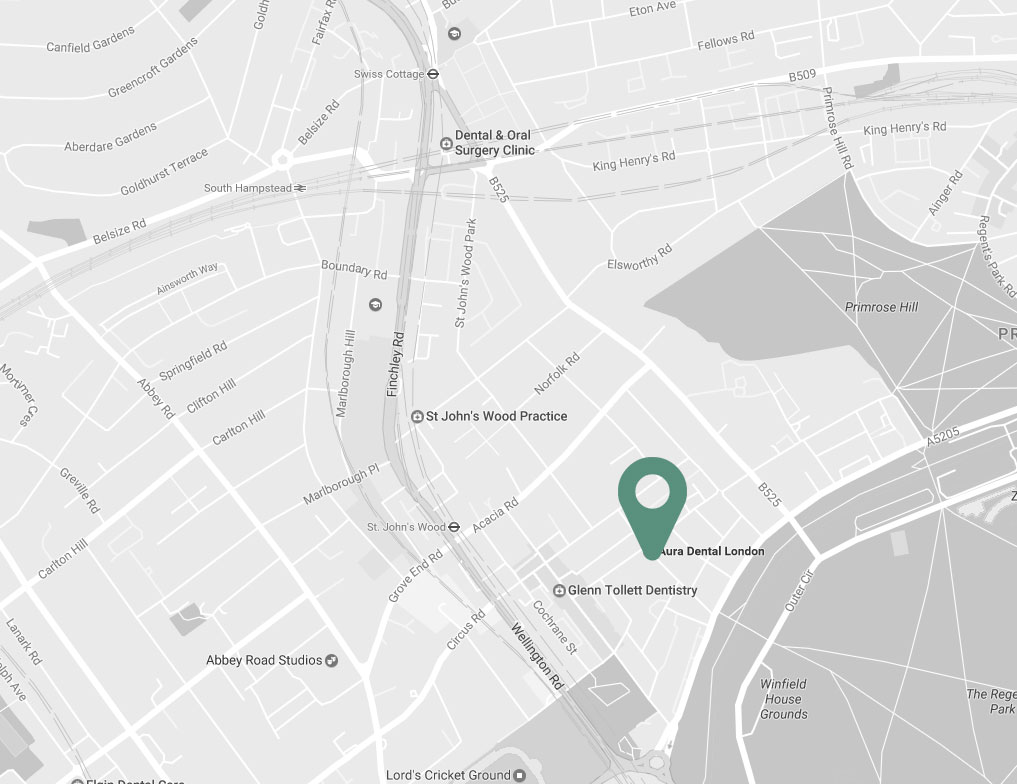

| Charlbert St, St John’s Wood London NW8 7BT |
|
| +30 6977 2099 88 | |
| info@naturopathy-med.com |