
Irritable Bowel Syndrome (IBS) is now being researched to the level of epigenetics and environmental factors. Such individual biomarkers can help in the creation of personalised nutritional treatment protocols.
Genetic analyses are becoming increasingly available to the public, making personalised plans more possible than ever. Digging deep at the molecular and genetic level for any chronic condition allows for more targeted treatments, and of course prevention. A recent study in Caucasian individuals found a link between genetic variations (in ZMIZ1 and TL1A) associated with impaired disaccharide digestion to IBS symptomatology. This result suggests that a nutrigenomic (the study of the effects of foods and food constituents on gene expression) approach for individuals with these variations, resulting in a tailor-made dietary plan, may greatly reduce IBS symptoms. The identified genetic SNPs (genetic variation) is responsible for reduced enzyme [sucrase-isomaltase (SI)] activity in the small intestine, leading to maldigestion of several carbohydrates (disaccharides like sucrose (sugar) and maltose). This could be the underlying cause of pain, cramps, diarrhea and bloating, as commonly reported by IBS sufferers, after consuming such foods. Researchers identified the specific SNP first by analyzing seven patients with IBS-D, as well as one asymptomatic relative from four families.
Findings were confirmed with a cohort of 1031 IBS cases and over 850 controls. The study confirmed that patients with rare congenital sucrase-isomaltase (SI) deficiency variations in the SI gene had a two-fold increase in IBS risk, as well as a significantly increased risk from a more common variation, 15Phe at SNP rs9290264. The study confirms the link between two genetic risk factors for IBS-D, both connected to disaccharide metabolism.
While these IBS sufferers would benefit from a low-FODMAP (fermentable oligosaccharides, disaccharides, monosaccharides, and polyols) diet, it may be unnecessarily restrictive if only disaccharides are poorly absorbed. Since not all IBS-D patients respond to the FODMAP diet, one should look at other underlying causes too.
Low FODMAP diets are popular among interventions for addressing IBS (pre-, pro- and synbiotics; non-absorbable antibiotics; diets (FODMAP, gluten-free). Foods rich in carbohydrates, especially high FODMAP ones, seem to be problematic in most IBS patients. A personalised approach is needed, as well, in order to address co-morbidities, food sensitivities, or other factors, as opposed to a “one size fits all” approach.
Fermentation of FODMAPs in the bowel produces gases such as carbon dioxide and hydrogen methane, among others, responsible for bloating and cramping. FODMAP digestion and gas production may slow bowel transit and eventually alter the microbiome, which can affect tight junctions (leaky gut) and activate the mucosal immune system, increasing the risk of autoimmunity and atopic conditions.
A meta-analysis linked a low FODMAP diet, as compared to a standard IBS diet, to significant symptom improvement. The study concluded that following a low FODMAP diet, with the help of a professional, could be a first-line approach to IBS management. Avoiding FODMAP foods and steadily reintroducing them can greatly help in minimising intolerances, as well as identifying food triggers, leading to a less restrictive diet. Since not all patients with IBS respond positively to a low FODMAP diet, the use of such genetic biomarkers can be shown to be very effective in identifying those who would most benefit.
References
Dolan R, Chey WD, Eswaran S. The role of diet in the management of irritable bowel syndrome: a focus on FODMAPs. Expert Rev Gastroenterol Hepatol. 2018:1-9. doi:1080/17474124.2018.1476138.
Eswaran S, Farida JP, Green J, Miller JD, Chey WD. Nutrition in the management of gastrointestinal diseases and disorders: the evidence for the low FODMAP diet. Curr Opin Pharmacol. 2017;37:151-157. doi:1016/j.coph.2017.10.008.
Lan X, Lan X, Chang Y, et al. Identification of two additional susceptibility loci for inflammatory bowel disease in a Chinese population. Cell Physiol Biochem. 2017;41(5):2077-2090. doi:1159/000475439.
Rodiño-Janeiro BK, Vicario M, Alonso-Cotoner C, Pascua-García R, Santos J. A review of microbiota and irritable bowel syndrome: future in therapies. Adv Ther. 2018;35(3):289-310. doi:1007/s12325-018-0673-5.
Varjú P, Farkas N, Hegyi P, et al. Low fermentable oligosaccharides, disaccharides, monosaccharides and polyols (FODMAP) diet improves symptoms in adults suffering from irritable bowel syndrome (IBS) compared to standard IBS diet: a meta-analysis of clinical studies. PLoS One. 2017;12(8):e0182942. doi:1371/journal.pone.0182942.
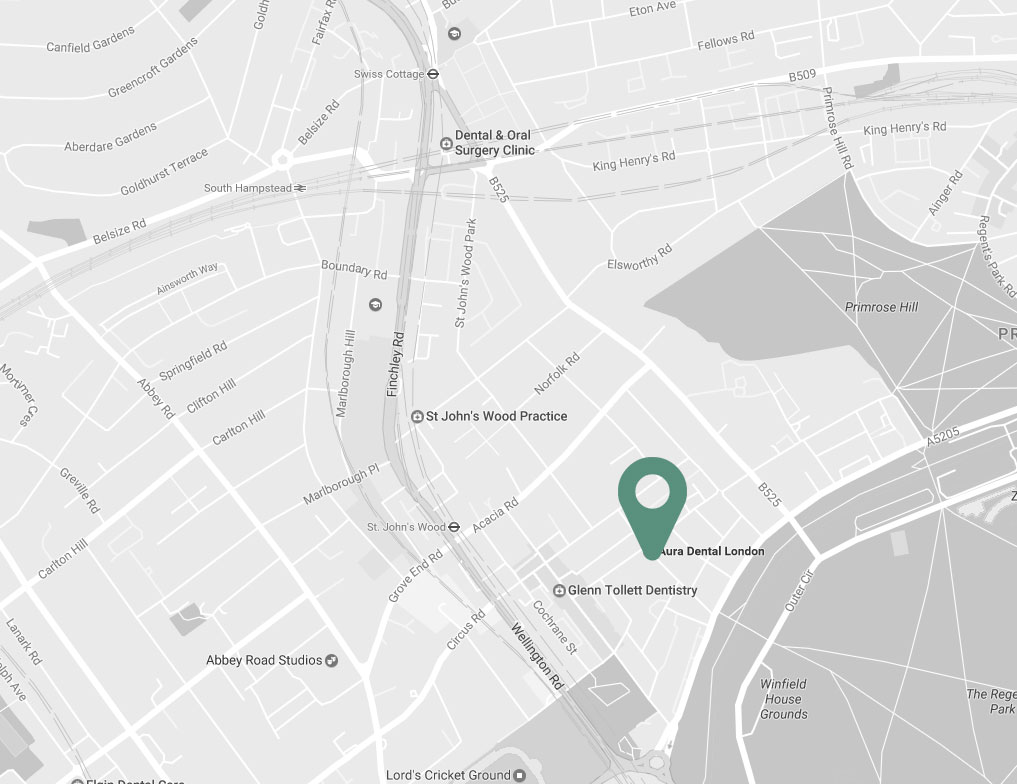

| Charlbert St, St John’s Wood London NW8 7BT |
|
| +30 6977 2099 88 | |
| info@naturopathy-med.com |